As the COVID-19 crisis unfolds one of its unique dynamics is the surge of new medical studies being rushed into print because of the extenuating circumstances of a global pandemic. To be crystal clear, these are studies produced using expert, scientific methodologies and conducted by credentialed epidemiologists and clinicians. But many have relatively small sample sizes and they’re being performed – many in China – under crisis conditions. So they don’t necessarily ‘prove’ things even in the limited way that larger, more organized studies can. But they’re giving us key information.
Let me point your attention to a few of them.
Because I’m not an expert on these matters in any way, I will keep my descriptions very general. If you want more information you can review the studies. In most cases, if you’re not a specialist, it’s easiest just to read the abstract.
*** One of the big questions about COVID-19 is its effect on children. The evidence is overwhelming that its impact on children is dramatically less than it is for adults, especially for elderly people. (Here’s a Times story on the general issue.) In general, young, healthy people do better with most diseases than older people. But the apparent disparity goes way beyond the general robustness of youth and appears to extend even to the very, very young who are often more vulnerable to diseases like the flu.
The question has been: do children actually contract the disease at a much lower rate or are they infected just as much or at similar rates to others but consistently present with much milder or even subclinical versions of the disease?
The difference may not have a major impact on the threat to children (here talking about under 20) but it could make a major difference in the degree to which children are a vector for the spread of the disease. This study published earlier this week, based on surveillance from Shenzhen, China suggests that children are just as much at risk of contracting the disease as adults. They are just far less likely to get severe cases. Key sentence from the abstract. “We further show that children are at similar risk of infection as the general population, though less likely to have severe symptoms; hence should be considered in analyses of transmission and control.”
Again, small sample sizes, rushed to print. None of these individual studies should be treated as definitive. But they are important pieces of the puzzle.
*** Another critical question is how deadly the disease is. People really want to know the answer to this question, for obvious reasons. As I noted on Wednesday there was a lot of bad reporting on the WHO’s announcement of a 3.4% death rate from COVID-19.
This number was not presented as an estimate of someone’s chance of dying as a result of COVID-19. We don’t know that answer yet and probably won’t in any definitive way for some time. It was the current percentage of identified fatalities per identified cases. That is a more specific and technical datapoint, highly influenced by the amount of testing.
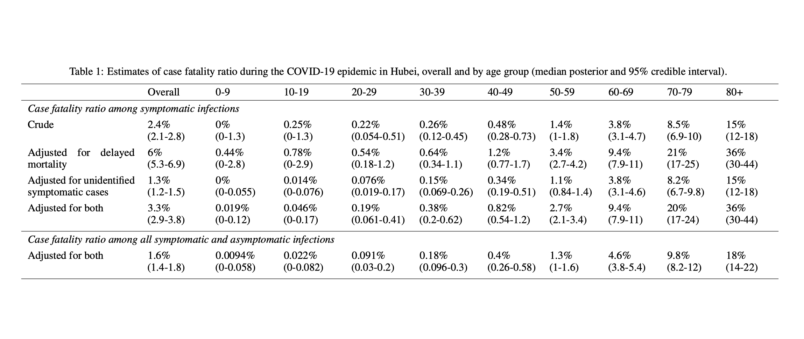
On Wednesday a new study was published based on the epidemic in Hubei from January 1st through February 11th. This study takes the official data and does additional modeling to try to get a handle on underreporting, transmission rates, etc. They came up with a 1.6% fatality rate. This was from an intense period of the epidemic in China. Fatality rates have been higher in Hubei than in the rest of China. Knowledgable experts have suggested we shouldn’t place too much focus on the 1.6% fatality rate – there are too many uncertain variables. What is more important is the age breakdown, which really drives home the threat to older people. See this chart.
As you can see, very low rates of mortality (relatively speaking for the young) up to very high ones for people over 80 and a steady slope from 1% on up over age 50. We have a great deal of evidence that for the great majority of people who are young or relatively young and in good health COVID-19 is a manageable disease. But for the elderly and those in fragile health it is very dangerous and deadly in a significant percentage of cases.
*** Another issue is smoking. It’s not a huge surprise that smoking might be a contributing factor to severity in a respiratory illness. But there’s significant evidence that smoking is significantly associated with COVID-19 progressing toward severe or critical disease. See this study from February 28th. There is also this study from February 26th which focuses on a gene expression found in smokers which is associated with COVID-19 – a “receptor” of virus. These findings may suggest that smokers are also more susceptible to infection. Key quote from the abstract: “In conclusion, our findings may indicate that smokers, especially former smokers, and people over 60 have higher risk and are more susceptible to SARS-CoV-2 infection.”
Note particularly here the “may indicate” phrasing. This second study is more tentatively connected to evidence from the course of disease in specific patients and should be treated as suggestive rather than dispositive.
I was struck in this case that this may apply even more to former smokers than current ones. But again, if you’re wondering about that all I can suggest is reading the study.