Arizona set statewide records on Monday for the number of new COVID-19 cases, hospitalizations, ventilators in use, and ICU beds in use, a range of markers that point to the severity of the ongoing outbreak.
In all, the Arizona Department of Health and Human Services recorded 2,392 new COVID-19 cases on Monday, according to data released today.
More worrisome from an epidemiological standpoint, however, is the state’s steady increase in hospitalizations and ICU and ventilator usage.
The state logged 1,506 COVID-19 patients in hospitals on Monday, setting another record, along with 340 ventilators in use and 502 ICU beds taken up by COVID-19 patients.
Dr. Murtaza Akhter, an assistant professor at the University of Arizona College of Medicine-Phoenix and a supervisory emergency physician at the Maricopa Integrated Health System, told TPM that the recent surge came as a surprise.
“COVID was here a couple of weeks ago, but nothing like at this level,” he said.
Akhter described to TPM an emergency department brimming with COVID-19 patients, the vast majority of whom had already tested positive and who arrived at the ER knowing what was going on.
“It felt like all hands on deck,” Akhter said, adding that he was “constantly” getting calls for incoming COVID-19 patients.
He added that “a couple of months ago, we were getting all of these stories about New York City — we had been prepped for a surge, but volumes went down.”
“I worked yesterday in the ER, and I was taken aback,” he said, recalling one patient who arrived and said her husband lay dead at their home, presumably also from COVID-19.
“The patients kept coming in, kept coming in,” he said. “There were people being diagnosed in the ER, and people who had already tested COVID-positive and were struggling to breathe.”
As a state, Arizona has begun to veer towards hitting capacity on its ICU and hospital beds. Governor Doug Ducey (R) issued an executive order in March mandating that hospitals create additional capacity for up to 50 percent more beds, and has said in recent days that the state would be able to rely on surge capacity to provide care for patients during the outbreak.
Local reports suggest the situation could be deteriorating far faster in hotspot areas.
In Tuscon, Dr. Steven Oscherwitz tweeted on Monday that his hospital had only one ICU bed remaining.
Just a #single #ICU #bed available this AM at Tucson Medical Center.
Better contact your #governor (quickly!)— Steven Oscherwitz MD (@drdetectve) June 15, 2020
Maricopa County, where the city of Phoenix is located, is in the hardest-hit portion of the state. The county reported huge case and hospitalization growth in a report released Monday, recording a total of 463 ICU admissions due to COVID-19.
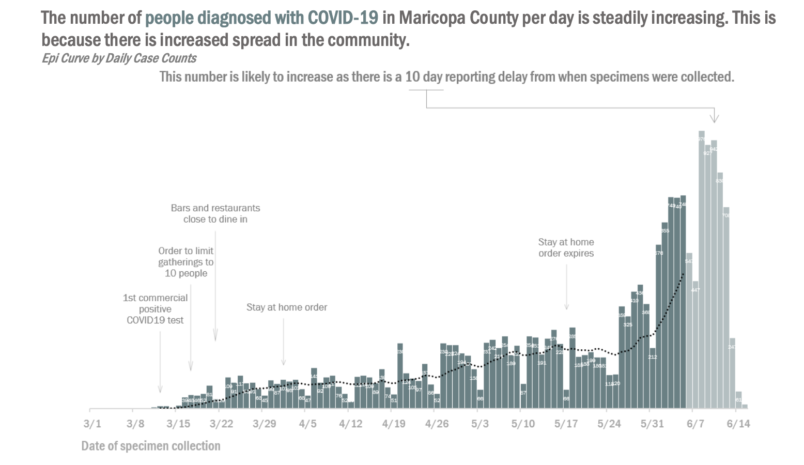
The state’s stay-at-home order was lifted on May 15.
Epidemiologists and public health officials have noted that Arizona’s case count began to increase sharply on May 25 — a long enough time after the stay at home order was lifted to suggest the virus has begun spreading widely again.
Akhter added that more cases were likely to come, in part because of the time it takes between infection and a patient falling into a serious enough state to require hospitalization.
“One thing we know about this disease is that there’s a lot of time from testing positive to decompensation,” he said.







Have mercy, it’s like something out of Stephen King’s THE STAND.
The GOP really REALLY wants that Senate seat.
Remember when Donnie said it would all go away when the weather warmed up? It’s 102 f. in Phoenix today.
thank goodness Trump didn’t hold his re-opening rally in Arizona. and i’m not sure why TPM is giving all the pub to Arizona. Florida is taking it in the shorts big time too.
Why doesn’t somebody make the difficult decision simply to stop all testing?!?