Traumatic brain injuries caused by blasts from improvised explosive devices is one of the most vexing and poorly-understood medical problems faced by soldiers returning from modern combat. Symptoms can range from coma and catastrophic brain damage to subtle but intractable changes in personality. Even mild TBI, the most common wound sustained by soldiers in the Iraq and Afghanistan conflicts, can leave injured veterans, their families, and their doctors struggling to cope. Current treatment options are limited, and the effects, including increased risk for neurological disorders like Alzheimer’s, can last a lifetime.
“There is still serious debate within the biomedical community about what exactly TBI is and how to treat it,” says Kevin Parker, head of the Disease Biophysics Group at Harvard’s School of Engineering and Applied Sciences and a major in the U.S. Army who has served two tours in Afghanistan. “Every patient is different.”
But imagine if it were possible to administer an antidote. Imagine if, immediately after an explosion, injured soldiers could receive a dose of medicine, perhaps through a device like an asthma inhaler, that would block the chemical process in the brain that leads to TBI. We might be able to avoid or reduce many of these injuries.
“That would be the dream,” says Parker, whose team of biologists, physicists, engineers, and materials scientists recently published a study taking a closer look at just what goes on inside brain cells–or neurons–when they are exposed to a jarring force like an explosion.
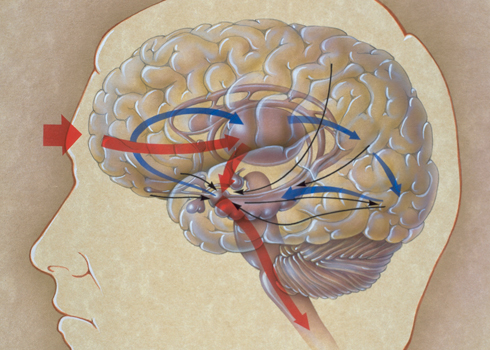
Until recently, conventional wisdom among many researchers held that TBI occurred when the force of a trauma killed brain cells. But Parker’s instincts and a study by Washington University researchers looking at brain images from actual TBI-sufferers suggested a different explanation: the cells weren’t dead; instead their axons–the branching appendages that connect them to one another–were badly damaged.
Using rat neurons, Parker’s team engineered a crude proxy for a brain (he calls it a “concussion on a chip”), simulated the force experienced during a blast, and observed what happened at a cellular level. They focused in on a group of proteins called integrins that serve as connectors between the inside of a brain cell and the outside. “They are like the bolts of the brain,” according to Parker.
Their experiments suggest that when integrins are bent or disturbed by a physical force like a blast wave, they initiate a complex chemical reaction that signals the neurons to retract their axons. Damage and swelling occur as the cells pull away from their neighbors–the same type of damage seen in patients with TBI.
Here’s the most interesting part: the team also found that treating the neurons with a compound that blocks one of the chemicals involved in the reaction within 10 minutes of the simulated injury reduced the damage.
While he cautions that the inhaler scenario is a long ways off, Parker is hopeful that further study on the chemical reactions triggered by a blast wave could eventually lead to more effective TBI treatments.
David Hovda, Director of the UCLA Brain Injury Research Center, is intrigued by the study and the possibilities it suggests.
“This paper really opens up a novel avenue from which to study how bio-mechanical events transmit themselves into intra-cellular damage,” says Hovda, who was not involved in the research. “I think this study could apply to all TBI, not just those from blasts.”
But he also cautions that it is a long way from a model in the lab to treating real people. “It is an exciting hypothesis,” he says. “It would be great to see some in vivo work next.”
Christine Hoekenga is a freelance writer based in the southwestern U.S. She’s written for High Country News, Technology Review, and managed online communities for the Smithsonian.
Have a story idea or tip for Idea Lab? Send them to Idealab@talkingpointsmemo.com